As many countries around the world, including our own, fight the COVID 19 pandemic, the medical profession, which is at the forefront of this fight, has suffered a rude awakening. As doctors, our efforts and thoughts are so focused on solving this problem that all other ailments have slipped down the priority list. And yet, as is usual in the professional life of a Neurosurgeon, the brain strokes, the head injuries (despite the lockdown), and of course the brain tumors and infections requiring emergency surgical intervention, keep coming.
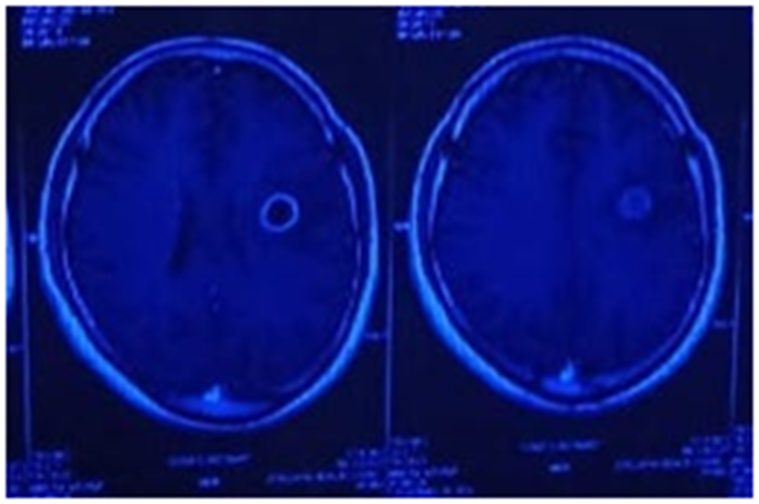
Ring enhancing lesion 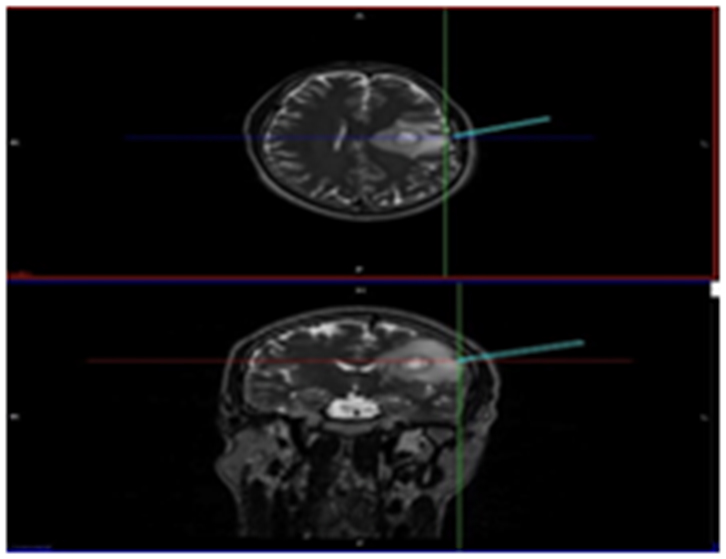
Tracker showing exact point of entry
Unavoidable and emergency neurosurgical procedures are carried out without waiting for the COVID 19 test in a dedicated and isolated environment where the medical staff members are required to wear complete Personal Protection Equipment kit (PPE) at all times.
Due to the persistently rising trend of Corona cases, as a thumb rule, all new admissions are treated as asymptomatic carriers and are treated as such. Non-emergency surgical procedures are carried out only after the COVID 19 test is found to be negative. This is for the safety of the patient, as if the Covid test is positive, surgical risk is higher. Even if the first test is negative, the surgical team members are required to don the complete PPE kit due to the added risk of aerosol born transmission of the disease.

Pre op registration for image guided surgery 
PPE ON
Data from around the world has shown that more than five neurosurgeons have succumbed to the Coronavirus as a result of infections picked up during surgical procedures, this is apart from fatalities in other medical disciplines. Safety for one’s own life, the most basic of human tendencies, does take precedence in such an unprecedented time. The surgeon must take a pragmatic view of the situation and deal with each case based on its merits and risks involved. While there is no other option other than emergency surgery in some cases, while others can be treated conservatively while ensuring there is no risk to the patient’s wellbeing.
I recently had a chance to treat a 26-year-old male patient who posed the same dilemma of conservative versus aggressive treatment with both having an equal chance of failure.
The patient had a sudden onset difficulty in speaking for 2 days. The MRI showed a ring-enhancing lesion in the left brain where the speech center is located. Differential diagnosis included a pus collection called abscess and a remote possibility of cancer. An abscess can be formed due to TB or any other type of brain infection and the treatment would vary accordingly. If the patient is not considered for the aggressive approach of surgery, I would have to consider the following two conservative approaches along with their aftereffects:
- If the patient is put on heavy antibiotics considering a non-TB infection, the patient may still end up having progression of the disease if it would be TB infection and also bear side effects of heavy antibiotics.
- If the patient empirically started on TB treatment, one would repeat the MRI only after 4-6 weeks to monitor the effects of the treatment, during which time if the treatment is incorrect, the abscess can grow fourfold.
With the Hippocratic oath in my heart, the thought of the risk of disease progression constantly in my head, and the life of this young man in my hands, I decided to be aggressive and perform the surgical procedure.
Stereotactic drainage of the abscess was the less favored option since it would require the patient to be transferred to the CT scan facility and back to the OT after fixing the frame on the patient, thereby risking exposure of multiple medical workers to a potentially asymptomatic COVID carrier.
Minimally invasive image-guided neurosurgery is the option I chose for the patient. This advanced modality gives a precise entry point to tap the abscess. Surgery was performed taking adequate precautions against potential infections. An incision of 3-4 inches was made at the designated position and 7-10 ml of the thick abscess was obtained area and sent for study. Within 24 hours’ diagnosis of TB was confirmed.
It was a great relief to get an exact diagnosis and not having to treat the ailment empirically.
The first MRI indicated a strong probability of a pyogenic infection which might or might not have been due to TB. The patient would have received broad-spectrum antibiotics which would not have helped him but would have affected his kidneys adversely.
My teachers implanted the principle in my brain that patient is and always will be the supreme priority for a doctor, no matter how adverse the situation.

